1. BACKGROUND
Patients visit the pharmacy many more times per year than their primary care physicians (PCP), with the community pharmacist having much more patient care time than their own PCP. This makes it easier for the community pharmacy team to detect medication-related problems (DRP), and through collaborative practice with the primary care team, any DRP that may arise can be addressed earlier.
2. CASE PRESENTATION
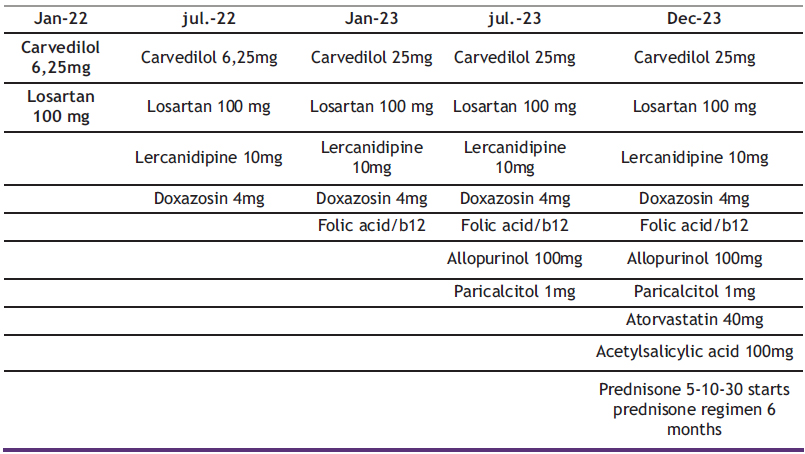
José, 82 years old, weight 87kg, height 179cm, non-regular customer of the pharmacy until 2023, diagnosed with hypertension in 2002, no other pathology. He does not smoke, drinks occasionally, does moderate physical exercise (walking) for 6-10 hours a week. He has no family history of hypertension, although he does have diabetes and inherited familial hypercholesterolemia. His blood pressure has been within range for quite some time, but he told us that since the summer of 2022 his blood pressure had risen and it was not enough with the medication he was taking at the time, adding his PCP lercanidipine 10mg and doxazosin 4mg (Table 1).
After several months in which the patient told us that he was not feeling well, we assessed his compliance with treatment, concluding that the patient was taking his medication correctly.
3. ASSESMENT
According to the guidelines of the Spanish Society of Nephrology, if resistant hypertension is suspected, a self-measurement of blood pressure (SMBP) is performed (Figure 1).
In the SMBP data we can see that blood pressure is slightly high throughout the day (SBP=145 mmHg, DBP=85 mmHg; Heart rate=87beats/min), with peaks of SBP=151 mmHg, DBP=87 mmHg, Heart rate=87 beats/min, with several drops in blood pressure not associated with the hours of taking medication (SBP=102 mmHg; DBP=58 mmHg; Heart rate=75 beats/min). It was therefore decided to refer the patient to his PCP by means of a referral letter with suspicion of primary hyperaldosteronism, a frequent cause of secondary hypertension and resistant hypertension, which entails an increase in vascular risk and organ damage related to both blood pressure and aldosterone levels (1).
4. TREATMENT
Therefore, a new blood test with aldosterone, calcium, sodium and potassium levels is recommended to his PCP (3).
June 2023: The patient went to the coast for a summer holiday, where he suffered an episode of hypotension and lost consciousness for a few seconds. He was transferred to Granada and underwent a complete blood test, obtaining high values of the aldosterone to renin ratio (ARR) ARR=46ng/dL, serum potassium 3.9mEq/L, serum sodium 139mEq/L, urine sodium: 143 mEq/L. Hypoparathyroidism was detected and due to the elevated ARR levels, an MRI scan was performed, showing a 2mm aldosterone-producing adenoma in the right adrenal gland.
Figure 1. Diagnostic and therapeutic process of resistant hypertension (2)
Table 1. Treatment evolution
5. OUTCOMES
December 2023: The patient is on the waiting list for surgical treatment of the adenoma.
The patient continues with the same antihypertensive therapy until the time of surgery, after surgery the new drug therapy will be evaluated.
6. DISCUSSION
Several published case studies echo the importance of community pharmacies in detecting medication-related problems (DRPs) and collaborating with primary care teams.
Similarly, in a case series published in 2023, one patient had a history of resistant hypertension for many years and had a negative initial assessment of secondary hypertension (including ARR). On re-evaluation, the ARF was close to the cut-off point and renin remained normal after prolonged strict drug washout, and further study of the PA demonstrated a unilateral aldosterone-producing adenoma that was surgically removed, resulting in complete biochemical remission and partial clinical success. Another patient was diagnosed with idiopathic hyperaldosteronism combined with obstructive sleep apnoea syndrome, which could increase renin leading to a negative ARR, and finally obtained a better therapeutic effect with PA-specific spironolactone as well as continuous positive airway pressure. Patient 3, with hypokalaemia as the main condition, was finally diagnosed with PA after exclusion of other diseases, and underwent laparoscopic adrenalectomy, with histological confirmation of an aldosterone-producing adenoma. Postoperatively, patient 3 achieved complete biochemical success without medication. The clinical status of all three patients was effectively managed, resulting in either complete resolution or notable improvement of their respective conditions (4).
José’s case aligns with existing literature, emphasizing the pivotal role of community pharmacists in early DRP detection, collaborative care, and the need for comprehensive investigations in suspected resistant hypertension cases.
It is important when screening whether or not a patient may have resistant hypertension, the patient’s control of their medication, since DRPs are one of the main causes of secondary hypertension.
Once the suspicion has been established, a referral should be made to their PCP, justifying our suspicions by means of the diagnostic tests available to us in community pharmacy. In this case AMPM or SMBP (ambulatory blood pressure monitoring) if a holter is available.
When determining the ARR, it should be borne in mind that there are many active ingredients that can modify the ARR, including antihypertensives themselves, but also non-steroidal anti-inflammatory drugs or even certain diets, which can lead to false positives in the diagnosis. It is in these cases that imaging tests, such as magnetic resonance imaging (MRI), can help define the diagnosis.
7. REFERENCES
Was the patient involved in a clinical trial? Please reference related articles
- Bonet Plá A, Dalfó i Baqué A, Domínguez Sardiña M, Egocheaga Cabello MI, et al. Self-measurement of blood pressure in primary care. Atencion Primaria. 2003; 31(8):545-552.
- Segura J, Gorostidi M. Hipertensión arterial resistente.En: Lorenzo V., López Gómez JM (Eds). Nefrología al día. ISSN: 2659-2606.
- Ares J, Goicoechea Diezandino M, Gorostidi M. Hiperaldosteronismo primario. En: Lorenzo V., López Gómez JM (Eds). Nefrología al día. ISSN: 2659-2606. Medicine (Baltimore)
- Jia M, Lin L, Yu H, Yang B, Xu X, Song X. Case series: Primary aldosteronism diagnosed despite normal screening investigations: A report of three cases. Medicine (Baltimore). 2023;102(20):e33724. doi: 10.1097/MD.0000000000033724.